GYNECOMASTIA SURGERY IN PARIS: CAUSES, PROCEDURE, RESULTS AND PRICE
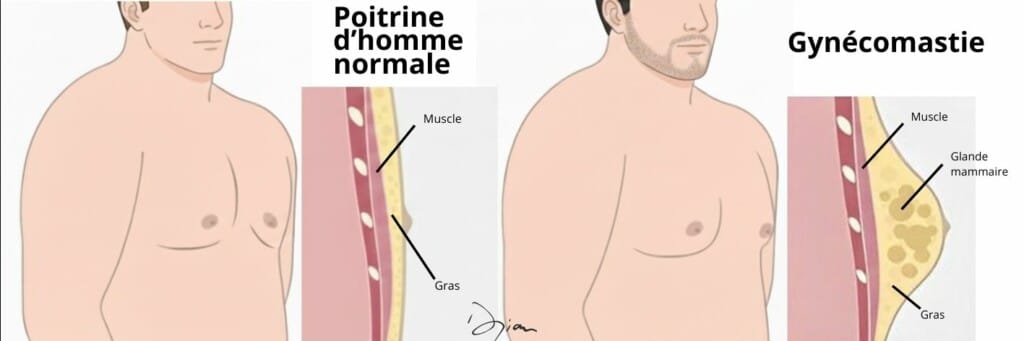
Hypertrophy breast, A feeling of discomfort in the chest, social discomfort: gynecomastia is excess breast volume in men, often linked to excessive development of the mammary gland, which does not always disappear with sport or weight loss. When this excess becomes a source of suffering, a cosmetic surgery This targeted surgical procedure helps to restore a more masculine torso. This guide details the causes, assessment, procedure, after-effects, results and price to help you make the right decision.
Your Questions
FREQUENTLY ASKED QUESTIONS ABOUT GYNECOMASTIA
HOW DO I KNOW IF MY GYNECOMASTIA CAN REGRESS NATURALLY OR IF AN OPERATION IS NECESSARY?
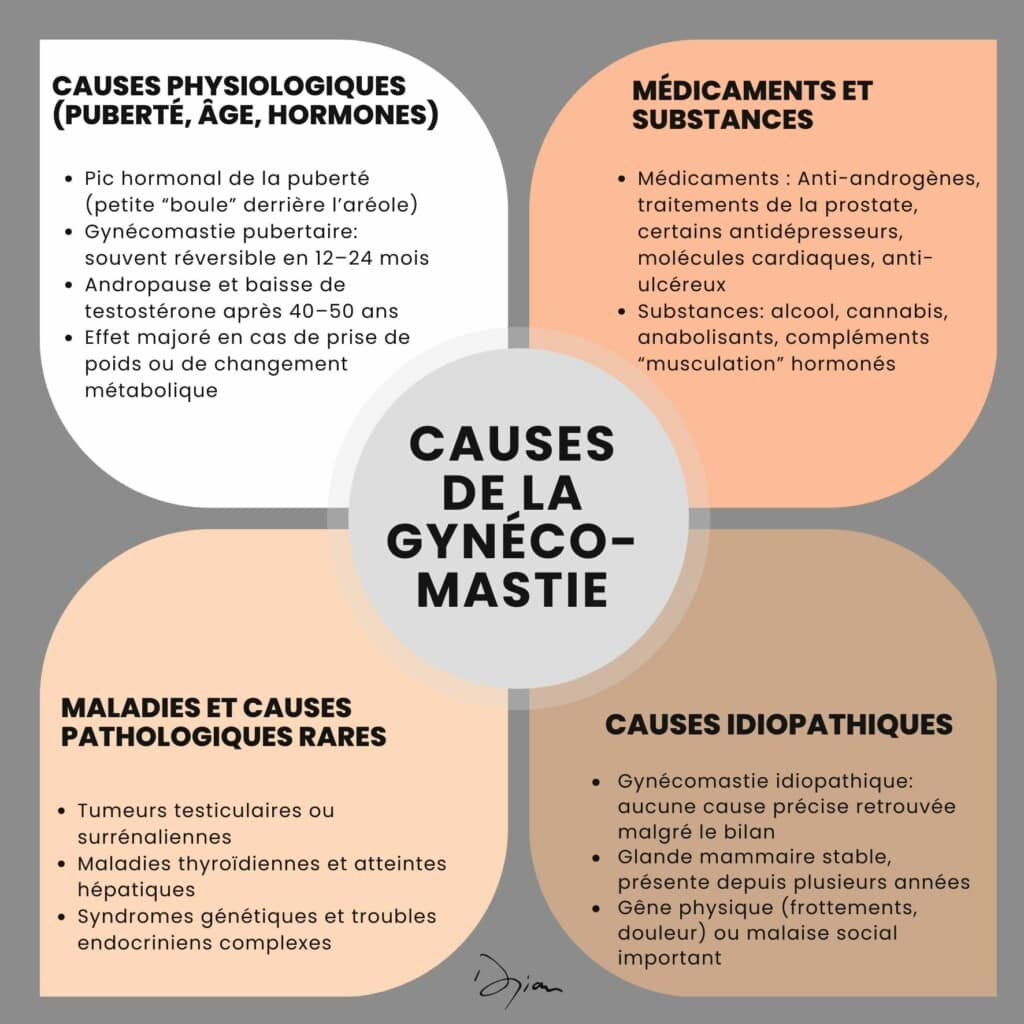
Gynecomastia that has only recently appeared, especially during puberty, can regress in one or two years. Conversely, a breast volume that has been present for several years, is stable and bothersome on a daily basis, and is unlikely to disappear without surgical treatment. The decision to undergo surgery depends on the patient's age, the length of time it has been present, the hormonal balance and the impact on social life. A specialized consultation is required to assess the appropriateness of gynecomastia surgery.
WHAT ARE THE MEDICAL CRITERIA FOR GYNECOMASTIA SURGERY?
The main criteria are :
- presence of a mammary gland confirmed clinically and on ultrasound
- real and lasting discomfort despite time or conservative measures
- Stabilized weight and absence of serious untreated cause
- State of health compatible with anesthesia
- Informed consent for procedures, scars and post-operative care
IS GYNECOMASTIA SURGERY PAINFUL AND HOW LONG DOES POST-OPERATIVE DISCOMFORT LAST?
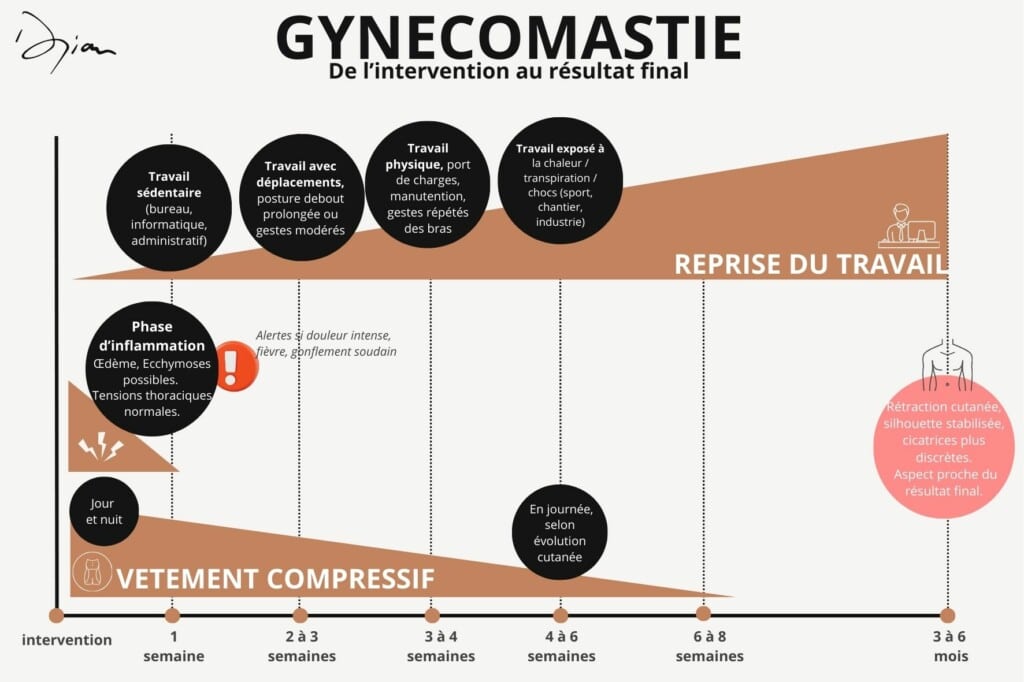
Gynecomastia surgery is rarely described as very painful. For the first few days, a tension and chest pain are frequent, but well controlled by prescribed analgesics. The most noticeable discomfort often comes from the compression garment, which is necessary for several weeks.
As a rule, daily life becomes fairly comfortable again within a few hours. ten days, although mild discomfort and local fatigue may persist for a few more weeks.
CAN GYNECOMASTIA SURGERY CHANGE THE APPEARANCE OF THE AREOLAS OR THE POSITION OF THE NIPPLES?
Yes, because breast volume reduction modifies areola support. In simple shapes, the areola often appears flatter and better integrated into a flatter torso.
In severe forms with In the case of excess skin, a real areola plasty can be planned: repositioning higher up, reducing diameter, symmetrization. These adjustments are intended to reinforce the masculine aspect of the torso. They are always explained before the procedure, with photos if necessary.
UNILATERAL GYNECOMASTIA: WHY IS ONLY ONE BREAST AFFECTED AND WHY IS SURGERY NECESSARY?
It is not unusual for one side to be more affected than the other., or even alone. Local differences in hormonal sensitivity, fat distribution or anatomy explain this asymmetry. The assessment aims to exclude another cause, particularly tumor, on the larger breast. If unilateral gynecomastia is confirmed and aesthetically troublesome, the operation can be performed on one side only, aiming for the most natural possible symmetry with the healthy breast.
WHEN DOES SOCIAL SECURITY REFUSE TO COVER GYNECOMASTIA SURGERY?
Social Security refuses to cover when it's essentially an excess of moderate volume with no functional repercussions, or of a request for purely aesthetic.
The absence of a significant mammary gland on ultrasound, an incomplete file or a “localized thinning” context mean that the procedure is classified as cosmetic surgery.
IS IT POSSIBLE TO CORRECT SIGNIFICANT GYNECOMASTIA WITHOUT A VISIBLE SCAR, AND WHAT AESTHETIC LIMITS SHOULD BE ACCEPTED?
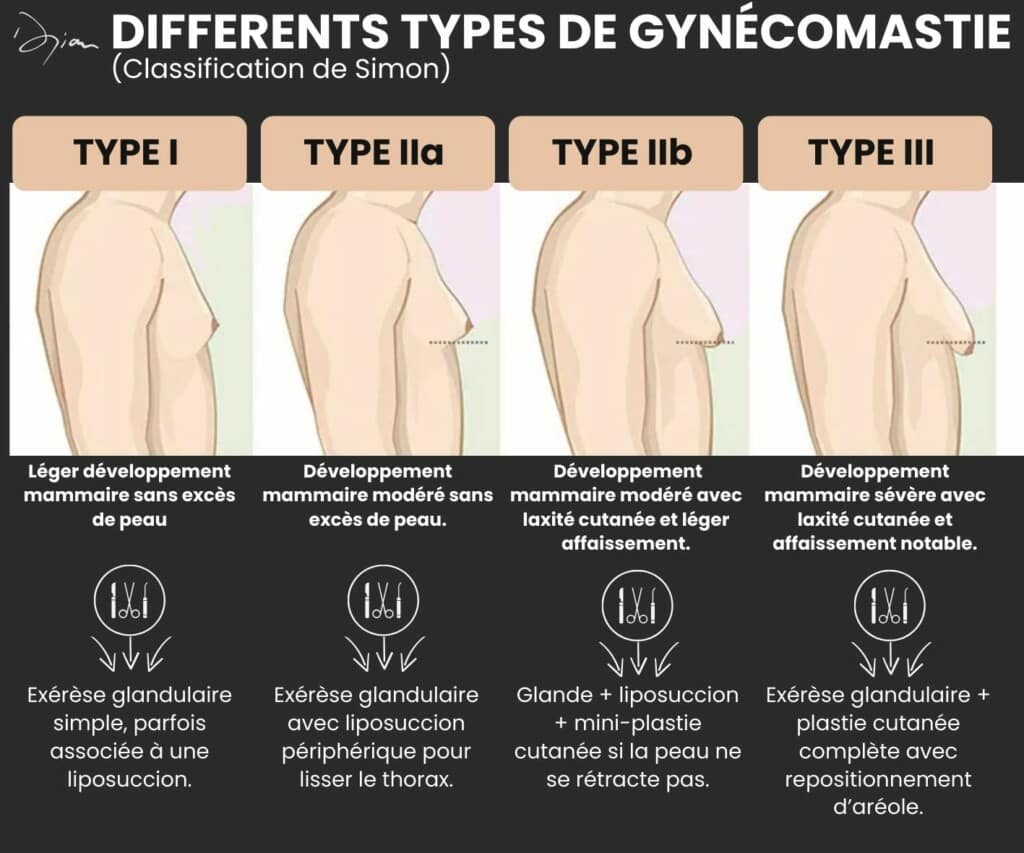
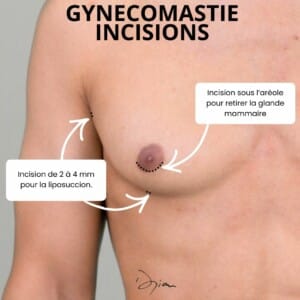
For moderate gynecomastia, The combination of liposuction and peri-areolar incision often offers an excellent compromise: effective correction of breast volume and very discreet scars.
For major hypertrophy with excess skin, wanting “no scars” isn't realistic: removing a lot of gland and skin imposes more visible marks. The real question becomes: what scar are you prepared to accept to regain a more masculine torso?
The surgeon will help you to consider this compromise in a clear-sighted way.
HOW TO DISCUSS GYNECOMASTIA AND THE IDEA OF SURGERY WITH THOSE AROUND YOU?
Talking to a loved one about gynecomastia often begins by describing the experience: embarrassment when undressing, avoidance of certain activities, impact on self-confidence. Explaining that it's a development of the mammary gland, and therefore a benign but real pathology, helps to move away from the register of “mere coquetry”.
Some patients choose to show the doctor's letter or the estimate in order to complete the project. Everyone is free to choose the degree of transparency they want: the important thing is to feel supported in the process.
YOU MAY BE INTERESTED
IN THESE SECTIONS
TO DR. DJIAN